Many people use ADD and ADHD interchangeably, but they are not exactly the same. If you’re wondering about the difference between ADD and ADHD, the quick answer is this: Attention Deficit Disorder (ADD) is a term now considered outdated, once described what is now recognised as Inattentive ADHD. This is which is one of the 3 types of Attention Deficit Hyperactivity Disorder (ADHD) where hyperactivity is not a primary symptom.
Understanding these terms is important, especially if you are seeking an ADHD diagnosis through the NHS or considering a private ADHD assessment. ADD is no longer a formal diagnosis under today’s medical standards, but it still appears in everyday conversations, online forums, and older research.
Throughout this guide, we’ll explore the key differences, symptoms, diagnosis processes, and treatment options for ADD vs ADHD. Keep reading to learn more and recognise the distinguishing factors between these terms.
ADD vs ADHD: Key Differences
The terms ADD and ADHD often create confusion, but understanding their differences is crucial. Attention Deficit Disorder (ADD) was once used to describe individuals who experienced inattentiveness without significant hyperactivity. Today, medical professionals, including those following the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders), no longer use the term ADD as an official diagnosis. Instead, it falls under the broader condition known as Attention Deficit Hyperactivity Disorder (ADHD).
ADHD is currently classified as a neurodevelopmental disorder that can present with inattentive, hyperactive-impulsive, or combined symptoms. The outdated term “ADD” referred specifically to what is now classified as Inattentive ADHD, characterised by symptoms such as forgetfulness, disorganisation, and difficulty maintaining attention.
This distinction is particularly important when speaking to healthcare professionals or seeking support through the NHS. While older adults might still refer to their struggles as “having ADD,” medical providers today use ADHD as the umbrella diagnosis.
Understanding this difference helps ensure that individuals receive the correct diagnosis of ADHD and access to effective treatment options, including Cognitive Behavioral Therapy or medication. You’ll get a closer look at symptoms and treatment pathways in later sections.
By aligning language with current standards set by organisations like the American Psychiatric Association, patients and professionals can better communicate needs, individualise interventions, and improve daily life for those living with this mental health condition.
If you’re exploring whether your symptoms align with ADHD, you can start by completing our free ADHD screening test. It’s a helpful first step toward understanding your needs.

Why Do People Still Say ADD?
Despite updates in medical terminology, many people, especially adults diagnosed decades ago, continue to use the term ADD. Historically, ADD gained popularity in the 1980s when the third edition of the Diagnostic and Statistical Manual (DSM-III) separated attention issues from hyperactivity. It provided a way to describe individuals whose primary difficulties involved inattention, forgetfulness, and poor executive function, without the classic symptoms of hyperactivity.
However, the release of the DSM-5 reclassified all presentations under the single name Attention Deficit Hyperactivity Disorder (ADHD), recognising that inattentive symptoms are just as impairing as hyperactive ones. In medical practice, the term ADD is now considered an outdated term, though it persists in everyday conversation, older websites, and among family members discussing past diagnoses.
The continued use of “ADD” also highlights the broader issue of public perception. Many still associate ADHD only with visible hyperactivity, overlooking the struggles faced by individuals with inattentive presentations. Raising awareness about the accurate definitions helps reduce stigma and promotes better understanding of mental health conditions like ADHD.
Types of ADHD
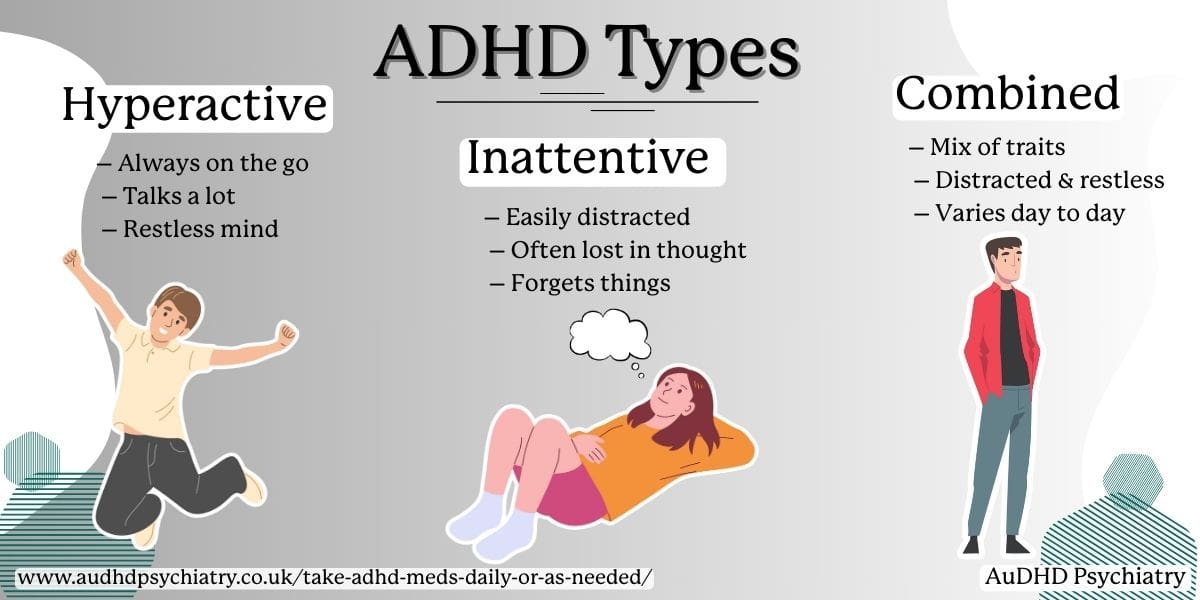
Today, ADHD is recognised as a condition with three distinct presentations, each affecting individuals differently. Knowing the types of ADHD is essential when seeking a diagnosis or discussing symptoms with healthcare professionals.
The three main presentations are:
1. Inattentive Type ADHD
This type is often associated with what people used to call ADD. Individuals may experience persistent problems with attention, organisation, and memory. Signs include frequent careless mistakes, being easily distracted, and difficulty following instructions. Hyperactivity is not a dominant feature.
2. Hyperactive-Impulsive Type ADHD
Here, symptoms of hyperactivity and impulsive behaviour are more apparent. Individuals may fidget excessively, find it hard to sit still, interrupt conversations, or act without thinking. This presentation tends to be more noticeable in young children, often leading to earlier referrals for assessment.
3. Combined Type ADHD
This is the most common form of ADHD and involves symptoms of both inattention and hyperactivity-impulsivity. People with Combined Type may struggle with executive function, emotional regulation, and time management, impacting their daily activities and relationships across different settings.
It’s important to remember that ADHD can evolve with age. For example, hyperactivity may lessen in adulthood, but issues like forgetfulness, disorganisation, and impulsive decision-making may persist. This complexity is why accurate assessment by an ADHD specialist is important.
Signs and Symptoms of ADHD
Familiarising yourself with the signs and symptoms of ADHD is an essential part of understanding this neurodevelopmental disorder. Generally, symptoms are under two categories: inattention and hyperactivity-impulsivity, though the way they appear can differ based on age and individual circumstances.
In school-aged children, ADHD symptoms often become noticeable when expectations for focus and behaviour increase. Teachers may observe careless mistakes, difficulty sustaining attention during tasks, frequent daydreaming, or trouble following instructions. Some children also display behavioral symptoms like fidgeting, excessive talking, and impulsive decision-making, such as blurting out answers before questions are completed.
In young children, symptoms can sometimes be mistaken for normal developmental behaviour. However, persistent signs such as constant movement, inability to engage in quiet activities, or extreme distractibility across different settings may indicate underlying ADHD.
For adults with ADHD, symptoms tend to shift. Hyperactivity often lessens with age, but difficulties with executive function, time management, organisational skills, and emotional regulation typically remain. Adults may struggle with maintaining focus during meetings, keeping up with daily tasks, managing responsibilities at work, and sustaining relationships. Missed deadlines, frequent forgetfulness, and feelings of being overwhelmed by routine activities are common. An AuDHD diagnostic assessment can help identify these challenges and provide clarity on treatment options.
ADHD can impact daily life at every age, interfering with academic achievement, employment opportunities, self-esteem, and mental health. It is important to understand that the severity and combination of symptoms can show up in many different ways between individuals.
For more practical help in managing these challenges, visit our How to Manage ADHD in the Workplace guide, which offers strategies and support options for ADHDers who want to thrive at work.
ADD Symptoms (Primarily Inattentive ADHD)
ADD symptoms are now understood to represent the inattentive presentation of ADHD. Individuals with this type of ADHD commonly struggle with attention, organisation, and memory, but without the pronounced hyperactivity seen in other types.
One of the hallmark signs is distractibility. People with inattentive type ADHD may find their minds wandering during conversations, lectures, or tasks. This may lead to careless mistakes, such as missing important details or forgetting instructions. Daydreaming is another common trait, particularly in children, who may appear disengaged even when trying to concentrate.
Forgetfulness can impact both personal and professional life. Misplacing items, missing deadlines, or failing to complete tasks are often daily challenges. Disorganisation may show up as cluttered living spaces, poor time management, and difficulty prioritising responsibilities.
Unlike those with hyperactive symptoms, individuals with primarily inattentive ADHD may not draw attention to themselves, making diagnosis more difficult. Teachers, employers, and even family members might interpret their behaviour as laziness or a lack of motivation, when in fact these struggles are rooted in a genuine neurodevelopmental disorder.
ADHD in women may also be harder to detect as they are more likely to exhibit inattentive symptoms. We recommend reading our guide on the Hidden Signs of ADD in Women for a deeper analysis.
Symptoms can evolve with age. In children, inattentiveness often leads to poor academic performance and social difficulties. In adults, it may contribute to career challenges, financial instability, and low self-esteem.
Recognising these symptoms of inattention is crucial for seeking timely support, improving self-awareness, and accessing effective interventions tailored to inattentive needs.
ADHD vs ADD Symptoms: Main Differences
Understanding the main differences between ADHD symptoms and ADD symptoms can clarify why certain behaviours are easier to spot, and why some individuals go undiagnosed for years.
As we’ve previously discussed, ADD symptoms, representing inattentive type ADHD. Executive function deficits are common, leading to challenges in setting goals, completing tasks, and regulating emotions.
In contrast, ADHD symptoms, particularly those involving hyperactivity and impulsivity, are more visible. These characteristics of ADHD tend to draw more attention from teachers, employers, and peers, leading to earlier referrals for assessment.
Here is a brief comparison of the two profiles:
| Feature | ADD Symptoms (Inattentive Type) | ADHD Symptoms (Hyperactive/Combined) |
| Main Challenges | Focus, memory, organisation | Activity level, impulse control |
| Visibility | Less noticeable to others | Highly visible to others |
| Common Issues | Daydreaming, losing items, missing details | Fidgeting, talking, interrupting, risk-taking |
Careless mistakes occur in both types but may have different origins: inattentive individuals might miss details due to mind-wandering, while hyperactive individuals may rush through tasks impulsively.
This distinction matters when seeking a diagnosis. Inattentive symptoms can be mistakenly attributed to anxiety, depression, or learning difficulties, delaying proper intervention. That’s why a structured evaluation, such as a neurodivergence assessment, is recommended if you notice persistent patterns impacting multiple areas of daily life.
ADHD vs ADD Diagnosis

How ADD Used to Be Diagnosed
The term Attention Deficit Disorder (ADD) was widely used to describe individuals who struggled primarily with inattention, without the pronounced hyperactivity seen in other cases. Diagnosis relied heavily on teacher observations, parental reports, and clinical interviewsk.
In the 1980s and 1990s, the diagnostic framework came from the DSM-III and later the DSM-IV, which allowed clinicians to categorise individuals as having either ADD (primarily inattentive) or ADHD (with hyperactive symptoms). However, understanding was limited; many individuals, especially girls and quieter boys, were missed because their inattentive symptoms did not cause obvious disruptions in class. Without visible behavioural problems, these cases were often overlooked or misattributed to emotional difficulties or lack of motivation.
Assessments focused largely on interviews and behavioural questionnaires, but formal testing tools were less standardised than they are today. Medical evaluations sometimes ruled out other mental health conditions or learning disabilities, but the process varied significantly depending on the clinician’s approach.
Because ADD symptoms often remained hidden, many adults today only receive a diagnosis after years of struggling with executive function, memory problems, or chronic disorganisation. Understanding how diagnosis has evolved helps explain why so many people are only now recognising their symptoms and why seeking a modern evaluation is important for accessing the right support.
How ADHD Is Diagnosed Now
Today, ADHD diagnosis follows a more structured and evidence-based approach, guided by the criteria outlined in the DSM-5. As we’ve mentioned, the term ADD is no longer used as a formal diagnosis. Instead, individuals are classified based on their presentations of ADHD: inattentive, hyperactive-impulsive, or combined.
Getting tested for neurodivergence involves a comprehensive evaluation process, including clinical interviews, standardised behaviour questionnaires, and input from family members or teachers when possible. Crucially, symptoms must have been present before the age of 12, persist for at least six months, and significantly impair functioning across different settings, such as home, school, or work.
Clinicians gather a detailed medical history, assess for coexisting mental health conditions (such as anxiety, mood disorders, or sleep problems), and may conduct a physical exam to rule out other causes. The first step typically involves speaking with your GP, who has the authority to refer you for an ADHD assessment via the NHS.
However, due to high demand and long waiting times, many people opt for private services. If you’re considering this route, our Top Private ADHD Assessment Services guide outlines trusted providers and what to expect.
Diagnosing inattentive type ADHD, what was once called ADD, requires careful attention to less obvious symptoms like daydreaming, forgetfulness, and chronic disorganisation. Without hyperactivity, these traits can easily be overlooked unless the clinician is experienced in recognising subtler signs.
Receiving an accurate diagnosis not only helps tailor treatment options, but can also enable access to important workplace accommodations through resources like Access to Work ADHD support. An informed and thorough diagnosis is the foundation for effective management, which can significantly improve outcomes at every stage of life. If you are considering getting evaluated, you can learn more about our private ADHD assessment process, which offers a structured, evidence-based approach.
ADD vs ADHD Medication
When it comes to managing symptoms, understanding the differences in ADD vs ADHD medication can be very helpful. While both conditions are now classified under the same umbrella diagnosis, individuals with predominantly inattentive symptoms may benefit from slightly different treatment options compared to those with more hyperactive-impulsive traits.
Stimulants remain the most commonly prescribed medication for all presentations of ADHD. Drugs like methylphenidate and lisdexamfetamine work because they increase the brain’s dopamine and norepinephrine levels, helping to improve areas like focus, attention span, and impulse control. These are highly effective for many individuals, whether they present with inattentive, hyperactive-impulsive, or combined type symptoms.
For individuals with primarily inattentive ADHD, clinicians sometimes prioritise stimulants that specifically target executive function and concentration, rather than those aimed at reducing physical hyperactivity. However, the choice of medication is always personalised based on symptom profile, side effect tolerance, and patient preference.
Non-stimulant medications offer another option, particularly for those who do not tolerate stimulants well. Atomoxetine, guanfacine, and clonidine are examples of non-stimulants that can support attention regulation without the side effects sometimes associated with stimulant use. These can be especially useful for those with coexisting mental health conditions, for example, anxiety or sleep disorders.
Routine medical follow-ups and checkups ensure that treatment remains effective and that any new challenges are addressed quickly. ADHD symptoms can shift over time, so a flexible, responsive treatment approach is essential.
To learn more about accessing these medications, you can visit our detailed guide on ADHD Medication in the UK, which outlines options, availability, and next steps after diagnosis. Finding the right medication is a collaborative process for you and your healthcare provider, ensuring that both symptom management and overall well-being are prioritised.
Treatment and Management of ADHD
An accurate diagnosis is just the beginning; the next crucial step is developing an effective treatment and management plan for ADHD. Thankfully, there are now various treatment options available that can help individuals with ADHD progress in their daily lives.
Therapy and Coaching
While medication can address many core symptoms, therapy and coaching are often key to mastering long-term ADHD management skills. Psychological support focuses on addressing patterns of thinking, behaviour, and self-esteem issues that medication alone cannot resolve.
Cognitive Behavioral Therapy (CBT) is widely known as one of the most effective approaches for ADHD. It helps individuals recognise negative thought patterns, reframe unhelpful beliefs, and develop healthier strategies for focus, time management, and emotional regulation. CBT is particularly valuable for improving executive function, which includes planning, prioritising, and completing tasks efficiently.
ADHD coaching is another supportive option. Coaches work collaboratively with individuals to set clear goals, build accountability structures, and improve organisation skills. ADHD coaching often addresses daily challenges such as planning projects, managing distractions, and sticking to routines.
Seeking professional help through therapy or coaching creates a space to explore personal challenges in a structured, non-judgmental environment. Whether addressing procrastination, low motivation, or emotional dysregulation, consistent therapeutic support can significantly enhance outcomes.
For many, combining therapy or coaching with medical treatment produces the best results, particularly when interventions are tailored to the individual’s daily activities and lifestyle demands. If you are exploring therapy options, consider looking for a practitioner who specialises in ADHD or executive function coaching to maximise the benefit of your sessions.
Other Resources and Tools for ADHD Management
Beyond medication, therapy, and coaching, many people living with ADHD benefit from using technology, apps, and community resources to manage their symptoms more effectively. These tools offer practical solutions for improving organisation, focus, and time management in everyday life.
Productivity apps such as Todoist, Trello, and Microsoft To Do can be especially helpful for individuals who struggle with executive function. These apps encourage users to break tasks into smaller steps, set reminders, and track their progress visually – a strategy that can significantly reduce overwhelm and procrastination.
Time management tools like Focusmate, Forest, or Pomodoro timers can help with sustaining attention for longer periods. These resources are designed to support individuals in building better work habits, creating a greater sense of accomplishment across daily activities.
Community support also plays an important role. Online ADHD communities, local support groups, and professional networks offer spaces where individuals can share experiences, exchange tips, and find encouragement. Feeling connected to others who understand the challenges of ADHD can greatly boost motivation and resilience.
If you are looking for practical options to supplement your treatment plan, our ADHD Resources & Tools page provides a curated list of helpful apps, strategies, and support platforms. Ultimately, effective management strategies involve a combination of medical support, personal resilience, structured interventions, and community backing, all tailored to an individual’s specific needs and goals.
ADD vs ADHD: Conclusion
Understanding the science-backed differences between ADHD and ADD is a great first step to seeking the right diagnosis, treatment, and support. While ADD once referred specifically to inattentive symptoms without hyperactivity, it is now recognised as Inattentive ADHD under the broader ADHD classification.
Today, ADHD is diagnosed based on structured criteria, recognising three presentations: inattentive, hyperactive-impulsive, and combined types. Treatment ideally involves a combination of medication, therapy, coaching, and the use of practical tools to support daily activities. Accessing accurate information and the right resources can make a significant difference in long-term outcomes.
If you believe you may be experiencing symptoms of ADHD, taking action is an important first step. We encourage you to book a private ADHD assessment to gain clarity, explore treatment options, and receive personalised support aligned with your needs.
Early intervention can help you build the tools and confidence needed to thrive at any stage of life.
Get clarity on private child ADHD assessments and the things most people don’t know by reading our guide: Private Child ADHD Assessment: What You Don´t Know.
Reference
Levick, C. (2024, November 4). How can a naturopath support ADHD? | Perpetual wellebing. Perpetual Wellbeing. https://www.perpetualwellbeing.com.au/understanding-adhd-and-the-role-of-the-naturopath/
You Might Also Like
Contact Us
We’re here to answer any questions you might have.
Get in Touch
Opening Hours
Contact Form
We’re here to help. Reach out and we’ll get back to you within 24 hours (Monday – Friday).




Leave a Reply